A White Paper produced by Connect Health’s Medical Director, Dr Graeme Wilkes
As Medical Director for Connect Health, who have 17 community NHS MSK contracts, ranging from physical therapy to chronic pain management, I am accountable for the care of over 300,000 NHS patient referrals per year provided by almost 300 clinicians: predominantly Physiotherapists but also Rehabilitation Therapists, Occupational Therapists, GPwSI, SEM Consultants, Rheumatologists and Pain Consultants.
Exactly a third of our referrals via self-referral or from GPs are for back pain with or without leg pain (sciatica) which is 100,000 referrals per year.
The Chartered Society of Physiotherapists state: Cauda equina syndrome (CES) is a rare condition, occurring in one to three in every 100,000 people. Up to two people in every 100 with herniated lumbar discs may develop the condition.
Given nationally we are receiving roughly 6x the MSK referral activity of a large NHS Hospital Trust, pathways for management of this condition need to be clear and efficient. As a community provider we are reliant on each of our local emergency care/ secondary care centres to provide an integrated pathway. Given there are several hospitals covering each contract we have over 30 Trusts to link in with.
Case Histories November / December 2018:
- CASE-1 Patient attends GP with 4 weeks bilateral sciatica. Referred to a private Physio. Attends physio 2 weeks later and has developed urinary urgency – GP contacted by physio same day and GP agrees to refer to community MSK but uses routine route stating patient “needs an MRI “and no mention of urinary symptoms. Patient self refers one week later to ED with bilateral sciatica and urinary symptoms. Diagnosed with urinary infection (UTI) based on dipstick showing white cells and sent home with antibiotics. 10 days later develops urinary incontinence, is admitted. MRI suggests Cauda Equina Syndrome (CES), is operated on. Has to self-catheterise post-op.
- CASE-2 Patient referred by GP routinely to community MSK with 4-week history of bilateral sciatica. Triage clinician calls patient three days later concerned re bilateral sciatica based on NICE suggesting this is a red flag in 2018 and finds that the patient has now developed urinary symptoms but not reacted to this as not counselled by GP. Sent to ED. Urgent MRI leads to emergency spinal decompression next day.
- CASE-3 – occupational physio calls patient at home with bilateral sciatica following Connects internal campaign on bilateral sciatica red flag awareness. Further explores symptoms and patient admits sexual dysfunction but “didn’t like to say”. Sent to ED. MRI performed – large disc prolapse, transferred to Neurosurgery and was decompressed that night.
- CASE 4 occupational consult of patient with bilateral sciatica for 2 months. Had developed urinary incontinence so occupational physio sent to ED with letter? CES. Diagnosed with UTI and discharged on antibiotics. Reattended physio and leg symptoms worse but no further incontinence. After discussion with senior colleague physio advised patient to go back to ED. Patient refused. Physio informed GP who stated nil else can be done except will refer to Neurosurgery routinely. Patient awaiting appointment counselled to re attend ED if further incontinence
- CASE-5 – patient with bilateral sciatica has 4 days of mild urinary urgency. Sent to ED by our APP – has a PR which is normal and is sent back to community for “MRI ASAP”. APP requests “MRI with urgency” though normal wait is 2-4 weeks. MRI performed 10 days later, shows a large central disc prolapse and is operated on that evening for CES.
Bilateral Sciatica
The above are all real cases that I became aware of in a 6-week period up to 31st December 2018. This came soon after being involved as Medical Director for Connect Health on a medicolegal case from five years ago where a patient developed Cauda Equina syndrome suddenly whilst slowly improving with bilateral sciatica and developed chronic bladder issues after emergency surgery. He had attended ED soon after onset of the urinary problems as he was well counselled and given he was improving prior to this catastrophic development in his life, we felt medico-legally we had done all we could, and it was just one of those things.
Medico-legal advice from the Medical Protection Society (MPS) was that the lawyers were (now) aware that Bilateral Sciatica was a significant red flag and advised we should be reacting to that. They were being advised by Mr Nick Todd, an eminent Neurosurgeon who happens to practice in my home town of Newcastle.
On further reading, I discovered that Mr. Todd has been a proponent of treating bilateral sciatica as a significant red flag deserving of emergency MRI scan and consideration of surgery. He has been promoting this additional approach for several years. He suggests that we are failing patients by only recognising the traditional signs of CES involving bladder or bowel or perineum or sexual function when the die is cast –i.e. it’s too late. Not always but enough to harm several patients on a recurring basis. This is articulated in his “White Flag” paper.
This is an opinion piece but based on a career of seeing such patients and is a must-read that you can download here:
Possibly more important for clinical practice and medico-legal aspects NICE have in their Clinical Knowledge Summary (CKS) in May 2018 added Bilateral Sciatica as a red flag for CES as covered in their statement here:
Having disseminated on Twitter that NICE guidance had indicated bilateral sciatica was a red flag, I was corrected by the Chair of the NICE Back Pain guidance committee that NICE did not have CES in their scope for their 2016 back pain guidance (incredibly!) and made no such recommendation. However, he acknowledged the CKS had stated this on their website in the publication above with the MPS. Strictly speaking, NICE currently have no guidance on CES.
As Medical Director I drew together my senior clinical team at Connect and we considered all aspects of where we were with CES:
- Our medico-legal insurers based on the current legal approach to CES were advising we considered bilateral sciatica a red flag
- Medical Protection Society and NICE had published in CKS that bilateral sciatica should be added as a red flag
- We were seeing bilateral sciatica cases within days or weeks or months declare themselves as Cauda Equina with potential patient harm resulting despite excellent counseling to attend ED if traditional red flag symptoms appeared – the standard approach.
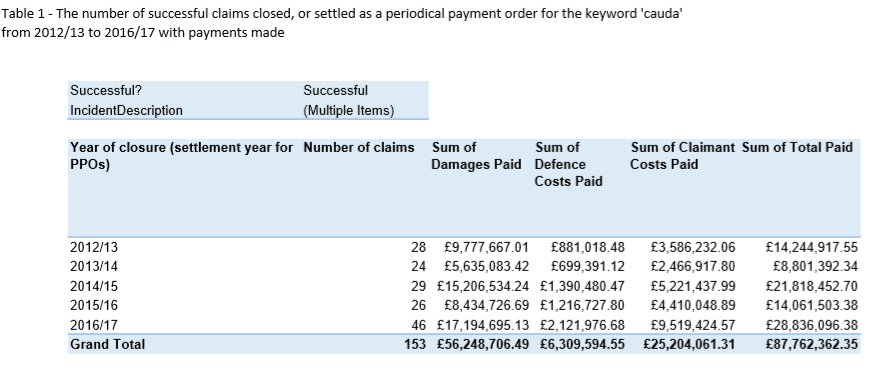
As part of our wide-search into this a Freedom of Information request to NHS Resolution (who manage all NHS provider litigation) revealed the stark facts that litigation for CES shows exponential increases in pay-outs from the NHS / taxpayer:
Almost £29million was paid out in the last year on record to April 2007 from £14 million in the previous year – more than double. Its almost two years on – I wonder where we are up to now?
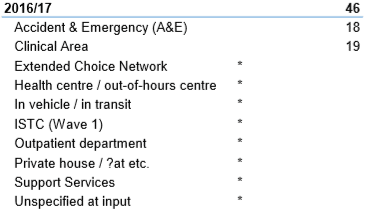
The pathway element subject to settlement of litigation with NHSR was documented in the last year on record as follows:
 *Indicates these sources had 5 or less
*Indicates these sources had 5 or less
Todd’s suggestion which would address this excessive patient harm and litigation is that
- Clinical signs have been shown to be unreliable at diagnosing CES – the PR exam has such a low sensitivity it is a waste of time
- Waiting for urinary or perineal sensory/ sexual dysfunction to appear is waiting for “white flags” – it is too late – damage has occurred whilst waiting
- Only an MRI can indicate true risk and a large central disc prolapse is the significant risk factor.
- Further debate is on the rationale for operating on such a disc as the majority will not go on to develop CES, but a significant number will, and some will be harmed.
As a result of the above, the Connect senior clinical team unanimously recommended a change to our internal guidelines for clinicians.
All felt patients are at risk of harm if presenting with bilateral sciatica. Rapid access to urgent same-day MRI is needed to add to the existing standard of that where traditional “red flags” are present.
Given none of our community services contractually have access to MRI with any urgency, the only option is to refer to hospital urgent care services. Guidance for management of Cauda Equina Syndrome physical therapy national pathways usually advises referral to the local ED rather than tertiary neurosurgical centres.
We initiated local discussions with all our receiving ED’s but found significant resistance to even entering discussions in some units. Where we started sending patients with bilateral sciatica (to departments we had communicated with on our intention) patients were universally sent out without access to urgent scan. Clearly this one red flag was not going to be entertained in Urgent Care.
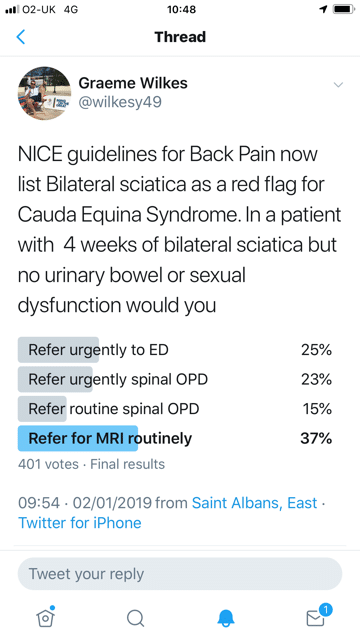
Given the issues, in an attempt to seek external opinion, I posted the following Twitter questionnaire in January to assess how clinicians manage bilateral sciatica with a significant 401 votes:
The clear outcome of this is confusion and varied practice! Given routine MRI in some parts of the country can by up to 10 week I am concerned that 37% of people would use this route for a “red flag”.
Since we started our debate at Connect and even since beginning this blog. “ Get it right first time” ( GIRFT) published their report on Spinal Surgery in January 2019
This includes a section on CES. Clear messages include:
- “The reliability of clinical diagnosis of threatened or actual CES is low and there should be a low threshold for investigation with an emergency MRI scan at the request of the examining clinician and MRI must be available at the referring hospital 24/7
- The decision to perform an MRI does not require dsicussion with the local spinal services.
- The MRI must be undertaken as an emergency in the patient’s local hospital and a diagnosis achieved prior to any discussion with the spinal services.
- The MRI must take precedence over routine cases and any reasons for a delay or a decision not to perform an emergency”.
A recent national audit – ENTICE (Evaluation of National Treatment and Investigation of Cauda Equina)20– collected data across 28 spinal emergency units in the UK. 4,441 referrals were made across a 6-month period (1st October – 31st March 2017). The study found that the SBNS/BASS standards are not currently being met, with potentially life-changing impacts on patients. Considering that 23% of litigation claims for spinal surgery in England relate to CES (based on GIRFT’s assessment of litigation claims in England between 2013/15 -15/16), this is unacceptable.
Poor compliance with the SBNS/BASS guidelines on managing patients with suspected CES appears to be driven by a lack of out of hours radiographer cover. Our recommendations are designed to encourage trusts to deliver timely access to MRI locally, removing the need for costly, and potentially risky, referrals between trusts.
The message above is clear and correlates with the 5 cases outlined above and our experience.
GIRFT did NOT consider or mention bilateral sciatica in this report. In a personal correspondence with the lead author, the opinion expressed was that the diagnosis of bilateral sciatica is subject to significant error and would lead to excessive emergency MRI scanning of conditions like spinal canal stenosis
What is clear to me is that:
- The provision of MRI scans for potential CES patients does not meet standards to meet patient safety requirements
- The reliance on a rectal examination to “exclude” CES is without evidence and should be abandoned as a screening tool giving false reassurance
- Patients with potential CES are being sent out from ED departments without adequate assessment (MRI). Patients returning to community services and often calling as they leave the ED places community clinicians in a very difficult situation and can lead to “second-best” pathways and potential litigation if CES develops/ progresses that will and does involve typically junior medical staff in ED, community clinicians and GPs.
- The debate on bilateral sciatica as a red flag and how this should be addressed is a complex one. I am informed and believe that the lawyers will have ample material to support malpractice from NICE CKS guidance and expert witnesses who are informing medico-legal opinion. The Medical Protection Society state this clearly here
As a doctor I signed up 34 years ago to “do no harm”. I have therefore led an excellent team of Connect Health clinicians to a new policy on suspected CES where:
- Updates on CES are provided in various media / formats / at in-service training
- Local discussions are occurring in all services with local ED
- ALL red flags suggestive of CES precipitate urgent referral to ED including bilateral sciatica
- An on-call rota of senior clinicians including myself has been instituted to advise our clinical staff and specifically pick up any patients sent home from ED whom we still have concerns about
- Audit of all out “suspected CES” is currently being processed and will occur quarterly facilitated by our live data warehouse
The GIRFT report outlines harm and potential harm to patients and we are spending in excess of £28 million public money on litigation for the sake of providing emergency MRI scans and operating on some significant disc prolapses that might not progress to CES.

 *Indicates these sources had 5 or less
*Indicates these sources had 5 or less